The Government’s Elective Recovery Taskforce has announced several actions aimed at increasing capacity in England in its implementation plan, especially through expanded independent sector involvement in the delivery of NHS services. While the measures, analysed in this article, represent an important acknowledgement of the need to urgently expand capacity and aspects of the plan can help ophthalmology if implemented effectively, to make a real difference policymakers must prioritise properly investing in NHS services and its workforce and infrastructure.
Summary of key measures
First announced in December 2022, the Elective Recovery Taskforce (ERT) last week published an implementation plan focused on expanding diagnostic capacity through greater involvement of independent sector providers (ISPs) in the provision of NHS care, alongside an announcement of 13 new community diagnostic centres (CDCs). The measures of particular relevance for ophthalmology are:
- Coordination and strategic planning of all available capacity over multiple years completed jointly at the integrated care board (ICB) and ISP level
- NHS England will ‘track monitor and evaluate independent sector’s impact on the long-term NHS capacity landscape’
- The Independent Healthcare Providers Network (IHPN) will conduct an annual benchmarking of training delivered in the independent sector
- 13 new community diagnostic centres, eight of which to be independent sector-led.
Better coordination and monitoring of ISP activity has potential to help ophthalmology
The ERT recommends that coordination and strategic planning of all available capacity over multiple years should be done jointly at the integrated care board (ICB) and ISP level, rather than between ISPs and individual trusts.
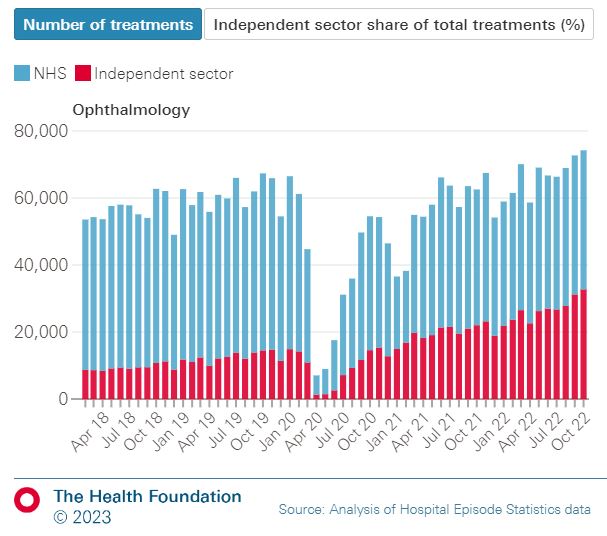
In ophthalmology, the number of NHS-funded cataract procedures delivered by ISPs has increased from around one-third pre-pandemic to half post-pandemic. As the Health Foundation showed in its recent analysis, this capacity has helped to bring down the cataract backlog. But this analysis also highlighted another crucial point – that more complex ophthalmology work is difficult to undertake in ISPs, and therefore as a priority we must tackle the chronic workforce shortages and underinvestment that NHS ophthalmology units face if we are to bring down outpatient backlogs and prevent avoidable irreversible sight loss.
While this ISP capacity has helped cut cataract backlogs, it has often been commissioned and delivered in an uncoordinated way, with little holistic consideration of the impact on NHS services, their workforce and the delivery of training. Indeed in our 2022 workforce census, a majority (58%) of NHS ophthalmology units reported that ISPs were having a negative impact on patient care and services in their area. The taskforce’s recommendation for joint planning between ICBs and ISPs therefore has the potential to support better approaches to the use of ISP capacity in ophthalmology. This aim also complements recent cataract contracting guidance from NHS England, which recommends that commissioners consider joint contracting arrangements where ISPs operate across several ICB boundaries.
The taskforce also commits to tracking, monitoring and evaluating the impact of the independent sector on long-term NHS capacity. This should help commissioners and clinical leads to tackle local challenges as they arise, and RCOphth will input into this process by sharing examples of what is working well and where there are problems that need to be addressed.
Recognition of need for more independent sector training opportunities is welcome, but delivery is the key
Another notable announcement from the taskforce is that the Independent Healthcare Providers Network (IHPN) will conduct a benchmarking exercise by October 2023 to measure the extent of training undertaken by ISPs, with a view to annual reviews which monitor progress.
We are pleased that the taskforce listened to the representations made by RCOphth on the importance of ISPs providing training opportunities when delivering NHS procedures, and this exercise should help commissioners and deaneries identify gaps in training provision across all medical specialties. In ophthalmology however, we already have extensive data demonstrating the issue – last month’s 2023 GMC National Training Survey found that just 8% of trainees who need training opportunities in the IS are able to easily access them. A 2022 survey of our Ophthalmologists in Training Group similarly found difficulties for trainees, especially those in the early years of training, accessing IS training opportunities – although for those that did, they rated the teaching quality and clinical supervision highly.
The focus for ophthalmology therefore needs to be on delivering, not just monitoring training. RCOphth is working closely and constructively with ISPs to improve the situation and will continue to do so, publishing last year a blueprint for delivering cataract training in the independent sector, after consultation with ISPs, training programme directors and ophthalmologists in training.
Additional community diagnostic centres need to support ophthalmology services
Alongside the publication of the taskforce report, Health and Social Care Secretary Steve Barclay announced 13 new community diagnostic centres, eight of which will be led by ISPs.
Community diagnostic centres can play an important role in tackling ophthalmology backlogs and the estimated additional 742,000 extra tests provided per year from these new CDCs would be welcome. As the largest outpatient specialty with a backlog of 650,000 patients, ophthalmology services must be included in this initiative. While recent reports of commissioners rejecting bids for ophthalmology CDCs are worrying, we continue to work with NHS England to ensure local commissioners are able to prioritise ophthalmology in the rollout of CDCs.
New community diagnostic centres that support ophthalmology services will need to be appropriately staffed with both ophthalmic technicians able to rapidly capture and analyse diagnostic data, as well as clinicians to provide clinical guidance and oversee services. Investment in and upskilling of the non-medical workforce – including ophthalmic image graders – can provide a relatively rapid increase in workforce capacity, working alongside ophthalmologists who will be designing, overseeing and delivering services. The Government needs to deliver on its commitment in the NHS Long Term Workforce Plan to provide a commensurate increase in foundation and specialty ophthalmology training places, alongside the existing funded commitment to increasing medical school places in the coming years.
Conclusion
Measures outlined by the government’s Elective Recovery Taskforce to better coordinate and monitor independent sector provision and training delivery have the potential to help ophthalmology services. This is because they may lead to more rational commissioning of services based on patient need and consideration of the overall impact on comprehensive NHS services. Detail is lacking though as to how this will be implemented.
Likewise the announcement of more community diagnostic centres could boost ophthalmology, but further information is needed on what the rollout will look like and how they will be resourced.
RCOphth will work with all stakeholders, including commissioners, ISPs and NHS England to ensure the implementation of these plans best supports the delivery of ophthalmology services. We will also continue to emphasise to policymakers the primacy of investing in NHS ophthalmology services and its workforce as the most effective way of creating sustainable services into the long term that can diagnose and treat patients quickly.